SEEING THE FRAILTY SYSTEM OF CARE in Midlothian
SHARING THE FINDINGS OF DISCOVER AND DEFINE STAGES
Background
Midlothian Health and Social Care Partnership are forging a path to change frailty identification and management. The journey began by using existing Primary Care records to stratify the population in Midlothian using the eFrailty Index (eFI), and this has led to new insights concerning the scale of the challenge of supporting citizens identified as living with frailty (~12,000 citizens). Through innovative partnerships with the British Red Cross and VOCAL (Voices of Carers Across Lothian), new ways of supporting people living with frailty and carers have been developed, which support people to navigate the system and access support to live well. Alongside this, Midlothian have developed new ways for health, care and third sector professionals to collaborate and work in multidisciplinary ways to identify people at risk and prevent crisis.
In order to push forward on this path of innovation, Midlothian Health and Social Care Partnership have successfully applied to the Technology Enabled Care (TEC) Pathfinder programme at the Scottish Government to fund the current project which seeks to explore how digital technology and design can act as transformation enablers. They have partnered with the Digital Health and Care Institute (DHI) to help them to use design-led approaches to engage with citizens and stakeholders and involve them in innovating the frailty system of care. The project benefits from strong clinician involvement, a range of key partners including the Red Cross and VOCAL, and robust senior management support.
THE CHALLENGE
Efforts to provide integrated and patient-centred care across disciplinary and sectoral boundaries have to-date been hindered, rather than enabled, by technology. There is currently no means of integrating effort and information across our care system – including statutory, third sector, and citizen held domains.
This lack of integration and data sharing impacts on the experiences of people living with frailty and their informal circles of care.
Project Aims
The aims of the project are to:
Improve the experience of care and support for people living with frailty, their family and carers, and staff;
Develop safe and highly reliable systems and pathways of care processes;
Breakdown the structural barriers between the organisations within the Health and Social Care Partnership and in our partnerships with external groups we need to collaborate with to deliver the change needed;
Achieve this in a way that starts with scale in mind.
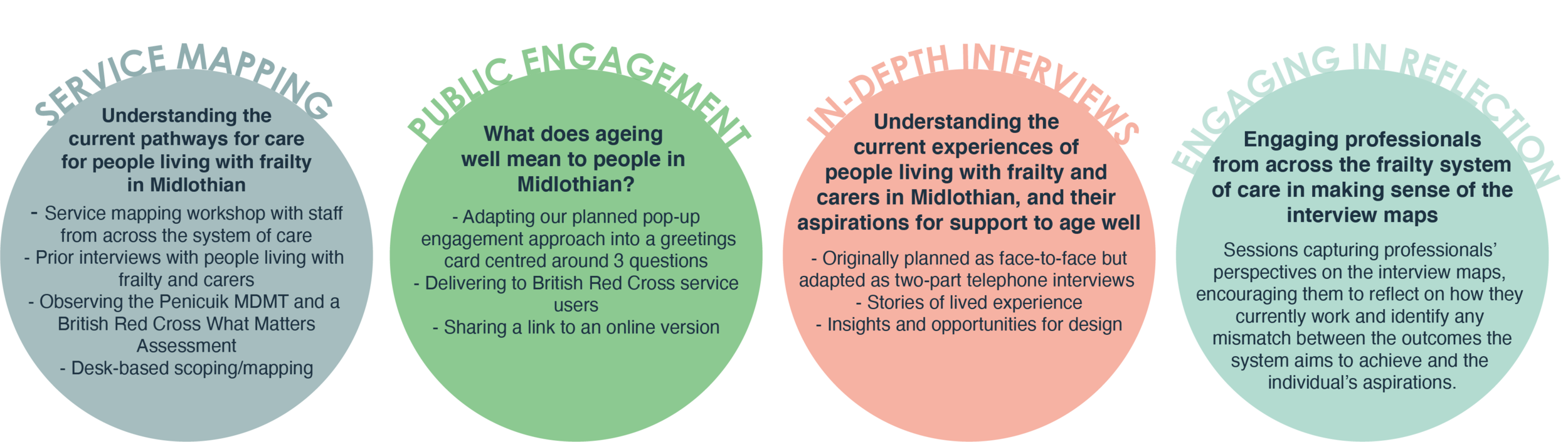
APPROACH
The TEC Pathfinder programme requires that all funded projects follow the Scottish Approach to Service Design. This aims to ensure that the people of Scotland are supported and empowered to actively participate in the definition, design and delivery of their public services (from policy making to live service improvement). As partners in the DHI, the Innovation School at The Glasgow School of Art enable active participation using specialist expertise in participatory design approaches to creatively engage stakeholders in reimagining the frailty system of care. Our approach is always bespoke to the context, the stakeholders and the challenge being explored.
Within this project we have used a range of bespoke engagements to bring different stakeholder groups into the design process. We needed to understand the current system of care from these different perspectives. We also wished to engage with older people more widely to understand how we can take a preventative approach to frailty and support self management of ageing.
The original plan was adapted due to the COVID-19 pandemic, with planned pop-up engagement in public spaces redesigned to facilitate remote engagement using greeting cards and an online tool, and in-depth interviews with people living with frailty and carers taking place over the telephone. Prior to the pandemic, a system mapping workshop was held with multidisciplinary and multi-sectoral professionals who deliver services for frailty in Midlothian. Researchers also observed a multidisciplinary frailty meeting and a British Red Cross ‘What Matters?’ frailty assessment in a person’s home to understand how these innovations are supporting more integrated care, and how these collaborative ways of working could be enhanced. More recently, workshops with professionals have taken place over video conferencing, engaging their perspectives and thoughts on the experiences of people living with frailty and carers gathered from our in-depth interviews.
STAGE 1: SERVICE MAPPING
Through our service mapping workshop with professionals and observations, we built up a picture of the system of care for people living with frailty from the perspectives of the many different professionals involved. These activities highlighted the complexity of the system and identified opportunities to support both professionals and citizens to better navigate and co-ordinate care.
In preparation for our engagements with people living with frailty and carers, we have reviewed data gathered from previous local service evaluations and worked with colleagues to understand consultations that have already been undertaken around care for older people in Midlothian. Through this process we identified key remaining questions that formed the basis of our in-depth interviews.
In parallel we engaged widely with others working on the topic of frailty, and identified key publications, best practice and individuals to light our path.
















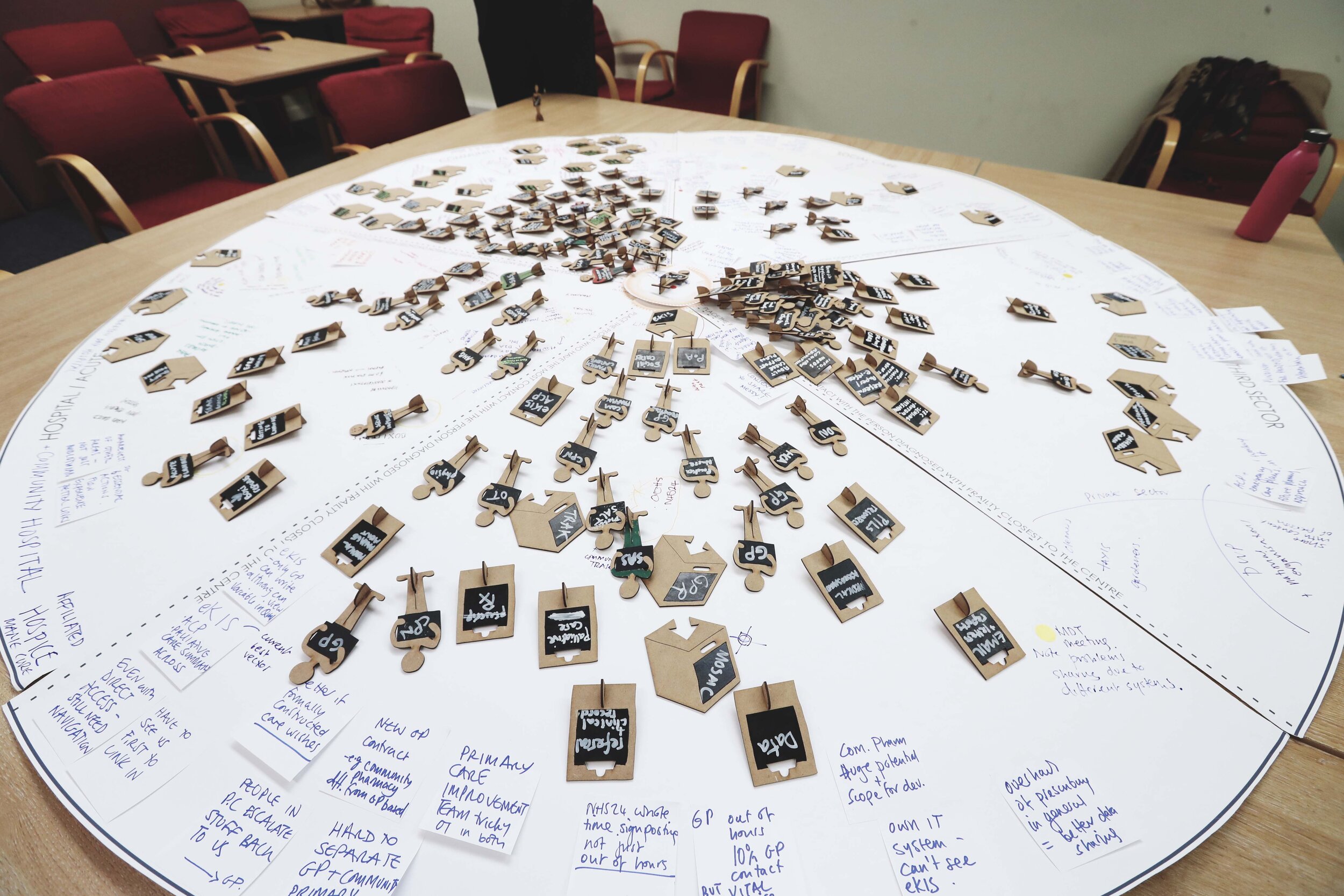
Images from a service mapping workshop in September 2019, all photography by Louise Mather, No Middle Name
FINDINGS OF SERVICE MAPPING
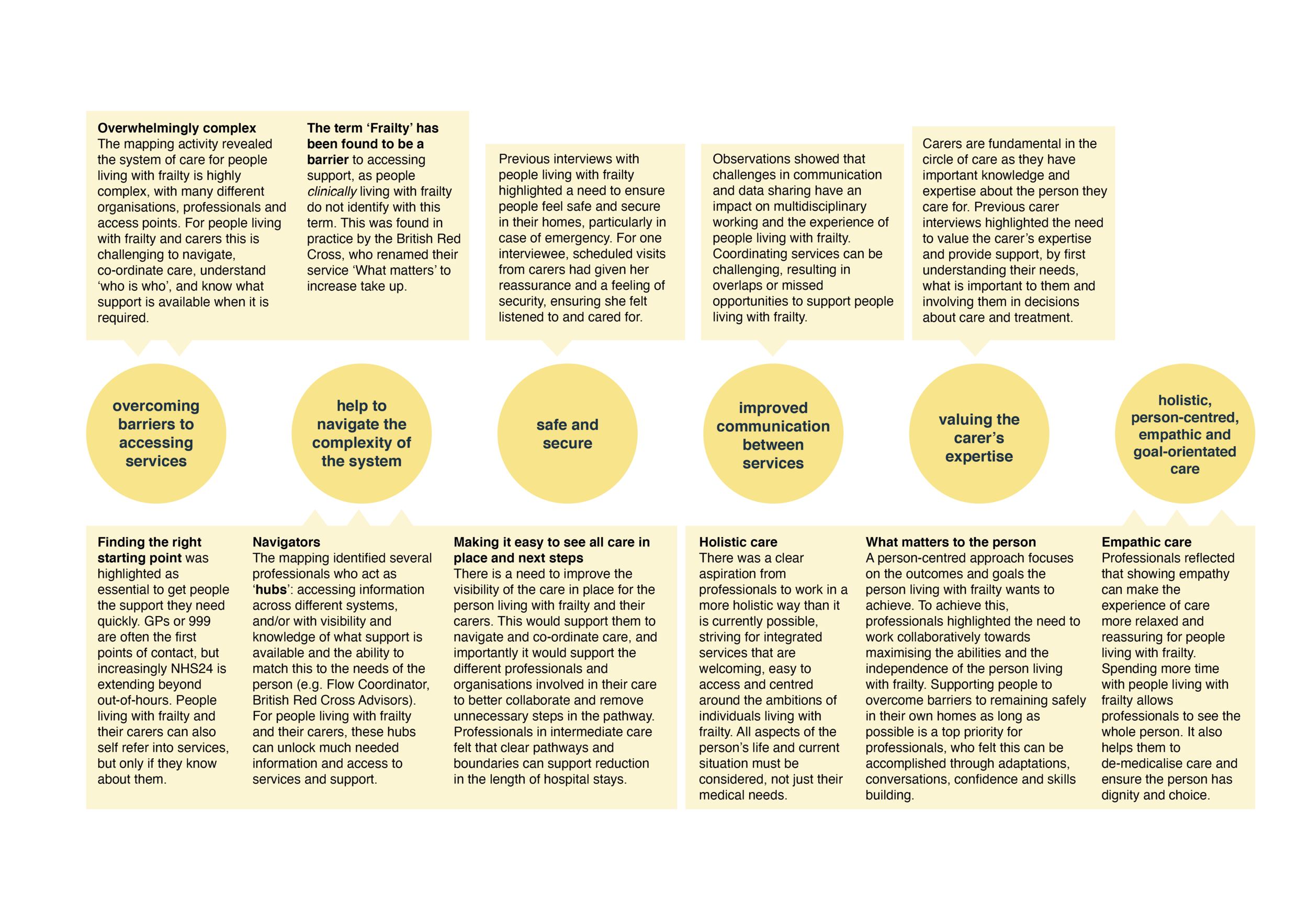
There were two overarching themes identified which reflected aspirations to innovate the current system of care to:
1) Improve the experience of accessing support for people living with frailty and carers
This theme gathered together all the requirements identified for improving experiences of accessing support, including the need for:
help to navigate the complexity of the system and the terminology used (i.e. ‘frailty’) by helping citizens find the people who act as navigators or information hubs;
improved communication between services;
valuing the carer’s expertise and involving them in decisions;
holistic, person-centred, empathic and goal-orientated care.
2) Improve multidisciplinary working and data sharing across the system
This theme reflected the ambitions of staff to change their ways of working and identified requirements for innovation to support collaboration and communication across the system, including the need for:
new ways of gathering consent and information governance to enable data sharing;
integration and collaborative working within statutory services and across sectors;
an ability to see what care is already in place and trusted, up-to-date information about the person in a timely and concise format.
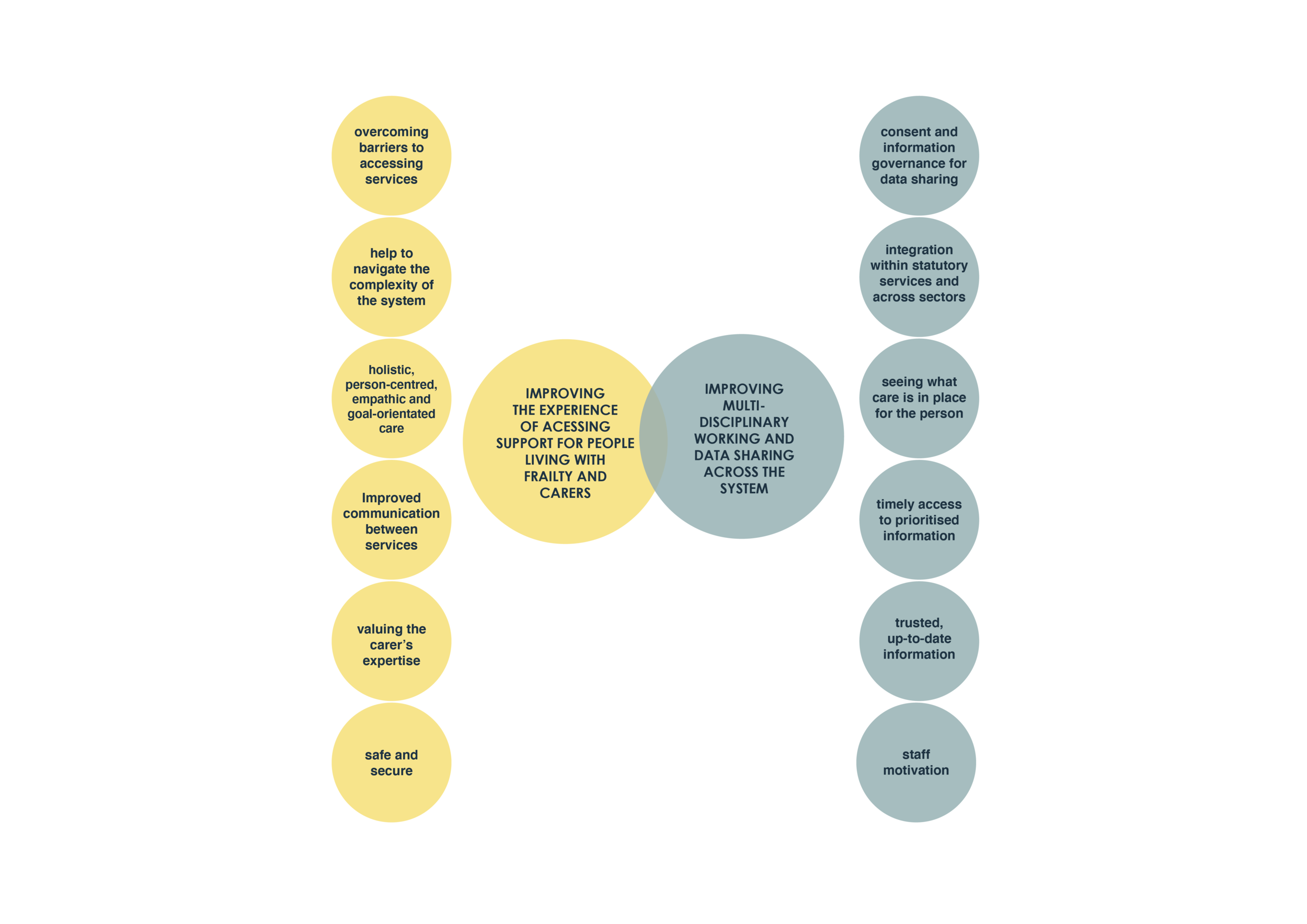

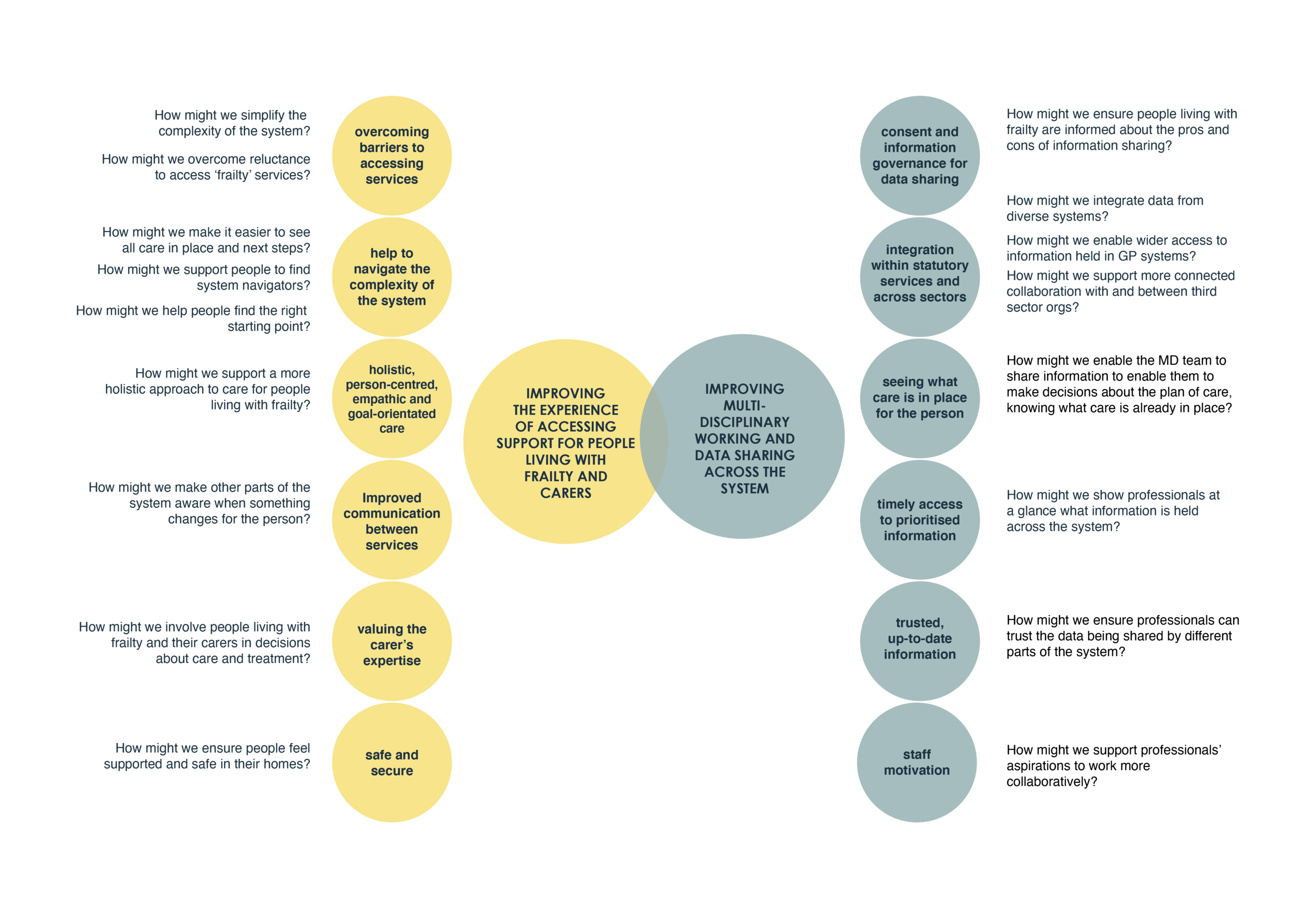
Images: Themes and sub-themes identified from the service mapping workshop, observations and desk-based research
STAGE 2: PUBLIC ENGAGEMENT
Our pop-up public engagement was scheduled to start when the first COVID-19 lockdown was imposed. We planned to pop-up in public spaces and events likely to attract older people living in Midlothian. Our engagement tool was designed to attract attention, using colourful flowers hanging on a trellis and a poster board giving information about the project. Each flower had an audio recorder which could capture individual responses to our first question, ‘What’s the best thing about getting older?’, and paper petals and leaves for facilitators to write down their responses to the questions, ‘What helps you to keep well?’ and ‘How can we support people to have positive experiences of getting older?’. The aim of the engagement was to start a conversation about ageing well, to understand:
What language should we use to engage people in services that can keep them well?
How do you engage people in self management to encourage a preventative approach to frailty?
Following the lockdown, we redesigned the engagement as a greeting card (see images below) using the same three questions. We also created an online submission form as an alternative to writing on the greetings cards. A link to the webpage was shared on social media. We sent out the greeting cards to 120 people living with frailty as part of British Red Cross packs. We received 17 returned cards. We also received 8 responses via the webpage.



Images showing the greeting card engagement tool (click through to see images of the front/back)
FINDINGS OF PUBLIC ENGAGEMENT
Responders valued the free time that comes with retirement and the freedom to decide how to spend it. There was also freedom in the confidence that comes with ageing and worrying less about what other people think of them. Many valued having children and grandchildren to spend time with, and taking pride in their achievements. Knowledge, skills and problem-solving abilities were also strengths of being older.
Getting exercise, being outdoors and eating well were strategies for keeping well. Some participants highlighted their dog or walking groups/friends as motivators to make outdoor exercise part of their routine. Many people wrote about the need to keep active and busy through crafts, reading, puzzles, learning languages or new skills. Being social and spending time with friends and family featured in most responses. Volunteering and caring for others were also mentioned.
Responders wanted more social activities and reasons to be active. They highlighted the need for more social contact, looking for opportunities to meet new people and particularly support people who are lonely or housebound. Some wanted more activities that were not stereotypically for older people. Volunteering opportunities, support to use technology, better transport infrastructure, and information about social activities were highlighted as areas of need.
A selection of responses from the greeting cards
STEP 3: IN-DEPTH INTERVIEWS
Interviews with people living with frailty and carers in Midlothian were designed with the aim of mapping the different kinds of support available in Midlothian from the perspective of older people and carers, to understand what people value now and in the future, and to identify any challenges or unmet needs. The interviews were designed in collaboration with project partners the British Red Cross and VOCAL. They helped to design the recruitment process to ensure we gathered the experiences of a diverse group of people living with frailty and carers.
The interviews were adapted to enable them to be undertaken over the telephone as a result of COVID-19. Telephone was preferred over internet enabled devices to ensure that participants did not need IT skills or an internet connection. The dial out feature in the Microsoft Teams platform was used to enable us to undertake three-person telephone interviews, with the British Red Cross Advisor or VOCAL Advisor joined by the GSA researcher and participant. For the majority of interviews, the GSA researcher managed the technical aspects, while the advisor took on the role of interviewer to ensure the participant felt comfortable talking to someone they already knew.
The interview was divided into two sessions, to enable us to produce two visual mappings following the first interview which were posted out to participants and used for discussion in the second interview.
Interview one: aimed to get to know the person and their interests and background, understand what care and support is currently in place, and understand what aspects of care they value most and why. It also aimed to understand any challenges they experience, and identify unmet needs they might have. We used the Place Standard Tool to prompt us to discuss life in Midlothian holistically.
Interview two: aimed to use the ‘what keeps you well'?’ and ‘circle of care’ maps (see below) to support the participant to reflect on their maps and identify anything missing or correct anything we had misunderstood. In some cases the British Red Cross or VOCAL advisor was able to suggest existing services, products, organisations etc which might help with challenges identified in interview one, and offer to make any referrals on behalf of the participant. We also used the circle of care map to discuss the participant’s views and concerns about information sharing between multidisciplinary and multi-sectoral professionals, and family and friends. In the final part of the interview we asked the participants about their aspirations for the future, and any support they anticipated needing to achieve these.
Nine people living with frailty and five carers took part in the interviews. We were not able to complete the second interview for one person living with frailty and one carer, but with their permission the insights they shared were included in the thematic analysis.


Images above show the ‘What keeps me well’ and ‘Circle of Care’ visuals for an interview participant who chose the pseudonym Georgina
ANALYSIS OF IN-DEPTH INTERVIEWS
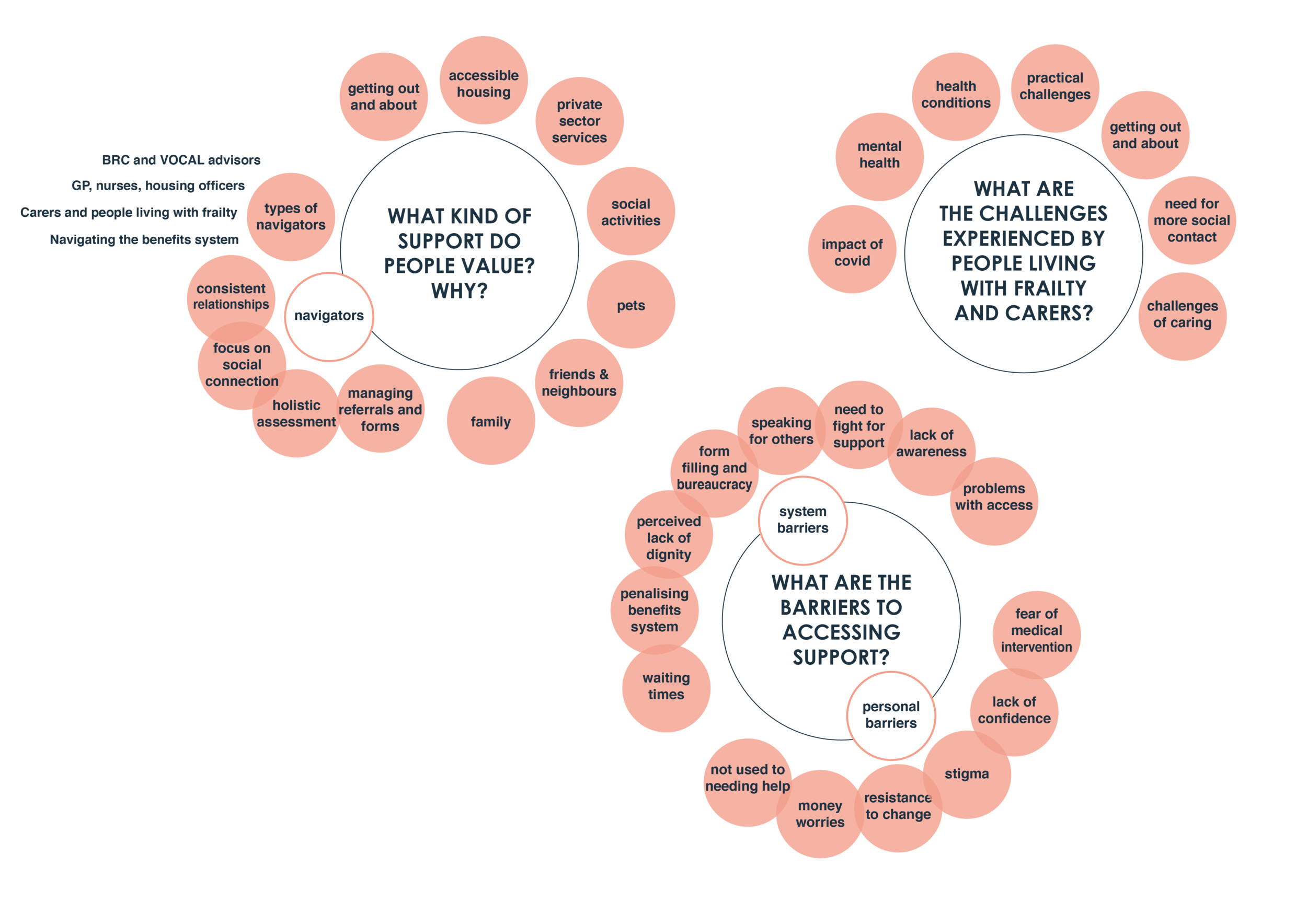
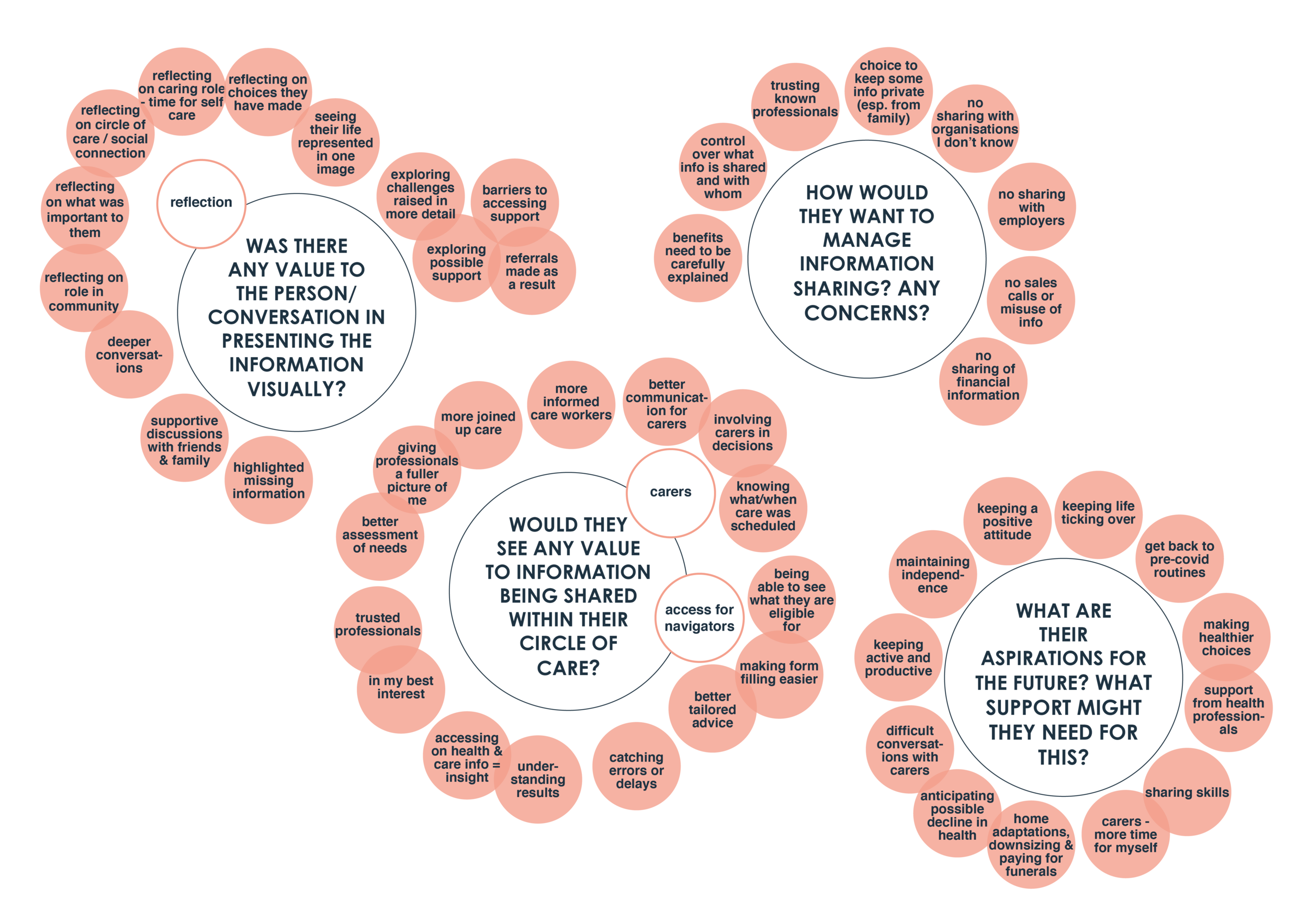
In addition to producing interview maps from each interview participant, we analysed the information gathered across the interviews to identify common themes. Our analysis set out to answer the following questions:
What kinds of support do people value, and why?
What are the challenges experienced by people living with frailty and carers?
What are the barriers to accessing support?
Was there any value to the person/conversation in presenting the information visually?
Would people living with frailty and carers see any value to information being shared within their circle of care? How would they want to manage this?
What concerns would people living with frailty and carers have about information being shared across the circle of care?
What are their aspirations for the future?
What support do they anticipate needing in the future?
Across all these questions we aimed to identify unmet needs, opportunities and ideas for new forms of support.
FINDINGS OF IN-DEPTH INTERVIEWS
The interviews uncovered a wealth of insight about the support people value, their personal challenges, and the system barriers that restrict access to support. Participants strongly valued help to navigate the complexity of the system and overcome barriers to access i.e. form-filling, knowing what support is available to them, and personal barriers such as not identifying as someone who needs help. Building up consistent relationships with professionals who used their knowledge of the system to tailor support to the person’s needs and manage referrals were seen as key to overcoming this.
The impact of covid-19 can be seen across the maps; for many, their hopes for the future were to return to normality and a more social and active way of life. The interview maps proved to be a useful communication tool to enable reflection, depth of insight and conversations about future aspirations and support they might need.
Participants were positive about the sharing of information about their care amongst the professionals who support them. It was felt this would enable better care by giving professionals a fuller picture of their needs. The need for a more joined-up approach to information sharing among health, social care and third sector professionals was highlighted as key to improving the co-ordination of care, particularly at times of transition. Participants also sought better ongoing communication from services about their or their loved one’s care, removing the need to follow up. There were some reservations about health information being shared with family, and concerns about commercial use of data and contact details. Most people wanted to be involved in managing what information is shared and with whom.
To see the detailed findings please request the ‘Interview Analysis’ document using the form at the bottom of this page. You can also request access to the individual interview maps in the document ‘Interview Maps’.
STEP 4: ENGAGING PROFESSIONALS IN REFLECTION ON THE INTERVIEW MAPS
We engaged professionals from across the frailty system of care in interpreting the interview maps, with each session focusing on a different interview participant. The sessions culminated in the generation of ‘how might we...?’ questions. In total we ran three group sessions and five one-to-one sessions with health, care and third sector professionals from a range of different disciplines. The sessions took place over Microsoft Teams video conferencing and used Miro to share visuals and record the discussion.
These sessions aimed to understand how the professionals responded to the maps, and capture their perspectives on some of the challenges and unmet needs highlighted. This aimed to offer a different lens on the interview maps, in relating the citizens’ challenges to the challenges of working in the system - and vice versa. The sessions also aimed to encourage the professionals to reflect on how they currently work, and use their knowledge of what is currently available to identify opportunities for new ways of working.
FINDINGS OF ENGAGEMENT SESSIONS WITH PROFESSIONALS
Professionals commented on the personal resilience shown across the maps, in how individuals cope with challenges and how they have adapted during the COVID-19 pandemic. They highlighted the reluctance of some older people to seek or accept help. In response, they identified a need to use asset-based approaches that focus on the resilience, knowledge, skills and contribution of people living with frailty, rather than just looking at their support needs.
Reflecting on the kinds of support people valued, professionals highlighted the time and space needed for good conversations to enable care to be designed around the person’s needs and aspirations. They asked how professionals throughout the system could be supported to feel they have time to have good conversations when they may feel under pressure to work quickly. In discussing positive experiences of professionals, carers and people living with frailty working together, professionals highlighted the importance of good communication between everyone involved in care. Professionals perceived the challenges relating to GP access as very difficult to solve. As the main starting point or ‘way in’ to the system, professionals highlighted a need to remove some of this burden from the GP’s role. Challenges with form-filling were discussed, and alternative ways of enabling more equitable and inclusive access were considered.
The maps led professionals to reflect that how they currently tackle system challenges can often contribute to the system’s complexity, with short- term funding leading to frequent changes. For some maps they highlighted differences between what the citizen valued and what the system identified as need, showing the need to centre innovation efforts around what citizens value.
TRANSLATING THE FINDINGS INTO ACTION
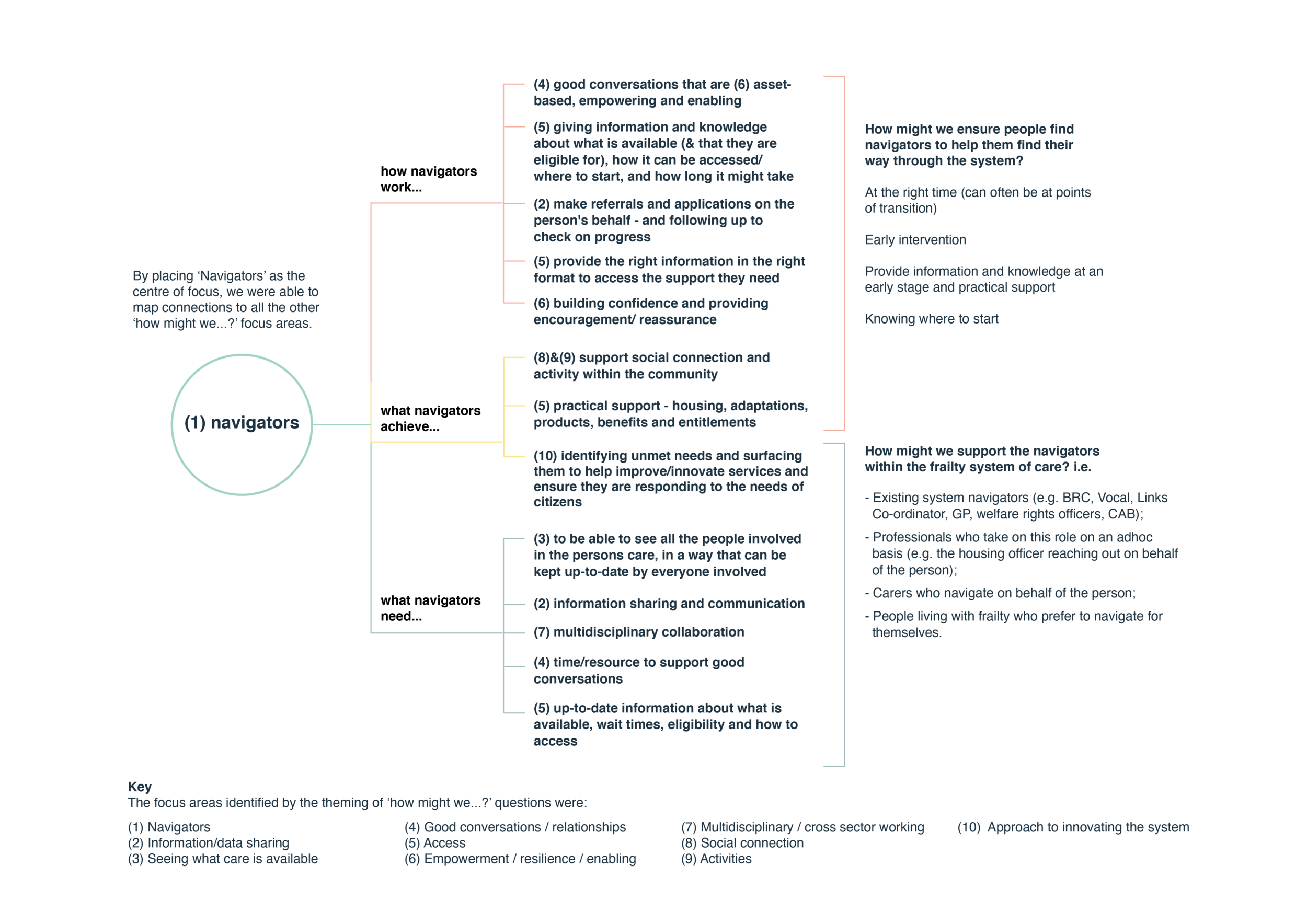
For each of the four stages we generated ‘How might we…?’ questions to translate findings into actionable insights. In a final stage of analysis we gathered together all the ‘How might we…?’ questions to identify clusters, and work with our project partners and steering group members to prioritise the key challenges to be taken forward as the focus area for the next phase of the project.
Image giving a visual summary of our approach to engagement, analysis and translation to define the challenge to be the focus area for the next phase of the project
FOCUS AREA
The findings and ‘how might we…?’ questions generated throughout the discovery phase highlighted the importance of system ‘navigators’ or ‘hubs’ to help overcome barriers to accessing support and help people living with frailty and carers to navigate the complexity of the health and care system.
We learned that valued system navigators can be:
Professionals with an existing remit to advocate and guide people through the health and care system (e.g. BRC and Vocal advisors, Links Co-ordinators, GPs, welfare rights officers, Citizens Advice Bureau advisors, link workers);
Professionals who take on this role on an adhoc basis (e.g. making a referral on the person’s behalf and following up or chasing to ensure they have received the support they need);
Carers who navigate on behalf of the person; or
People living with frailty who prefer to navigate for themselves.
Two overarching ‘how might we…?’ questions will guide our focus:
How might we ensure people find navigators to help them find their way through the system?
How might we support the navigators within the frailty system of care?

NEXT STEPS
We are now moving into the ‘Develop’ phase of the Scottish Approach to Service Design. This will involve working with people living with frailty, carers and professionals to develop ideas for ways of responding to the focus area and associated challenges identified.
REQUEST THE FINDINGS
Please fill in and submit the request form below to access the outputs of the in-depth interviews. We are keen to share the findings and understand how they are being used.
Further Information
For more information about this project please contact:
Matthew Curl, Matthew.curl@nhslothian.scot.nhs.uk
Cate Green, cate.green@dhi-scotland.com