TRANSFORMING CONVERSATIONS ABOUT TYPE 2 DIABETES
IN PARTNERSHIP WITH NHS LANARKSHIRE
Background
As part of a programme of work commissioned by the Scottish Government, the Digital Health and Care Institute (DHI) formed a strategic partnership with NHS Lanarkshire to collaborate on health and care service transformation. Diabetes was identified as a key area of need in consultation with the Chief Executive and the South Lanarkshire Health and Care Partnership’s Long-Term conditions group. Following further scoping activities with the NHS Lanarkshire Diabetes Service, services for people living with type 2 diabetes were identified as the focus for innovation and redesign activities. The project was undertaken between December 2017 and May 2019. Led by a team of design researchers from The Glasgow School of Art (GSA), the overall aim was to explore person-centred approaches to diabetes care in Lanarkshire and create a roadmap for future care, working together with those delivering the services and those receiving care.
FOCUS AREAS
Our early scoping work with specialist staff within the diabetes service in Lanarkshire identified a number of specific challenges relating to care across the interface of secondary and primary care, including the need for more support for primary care staff to improve the consistency of care. This is in the context of challenges as a result of discontinuation of the Diabetes Managed Clinical Network (MCN) and changes in the way that outcomes are reported by primary care following the end of Quality Outcomes Framework (QOF). These insights were supported by the findings of previous GSA research with people living with long-term conditions, which pointed to the importance of the diagnosis conversation in engaging people in self management. This supported us to identify two clear focus areas with associated research questions:
By focusing on one key moment in the care journey, i.e. the conversation between the primary care health professional and the newly diagnosed type 2 patient, we aimed to understand how secondary care and primary care staff could work more collaboratively to improve self management in the community and prevent referral to secondary care. Through exploring and mapping current care experiences and identifying aspirations for future care, we aimed to identify opportunities to redesign the type 2 diabetes diagnosis conversation to support early engagement.
We created a visual to communicate these focus areas, and show how they integrate with the overarching aim of person-centred care. The ‘donut’ model used primary and secondary care settings as a basis of understanding the current system of care, showing the person living with type 2 diabetes at the centre, with the interface between primary and secondary care depicted by frosting, and individuals involved in care as sprinkles.
‘Donut Model of Care’ Credit: Sneha Raman and Gemma Teal, 2018
PROJECT VIDEO
Video credit: Louise Mather, No Middle Name, 2019
METHODOLOGY
A participatory design approach was used to iteratively explore and ideate with a diverse group of participants including people with lived experience of diagnosis and health professionals in NHS Lanarkshire. This approach was used to integrate multiple perspectives to ensure that any innovation meets the expectations and needs of all those who provide and receive care.
Credit: Louise Mather, No Middle Name, 2019
INTERVIEWS with health professionals
We interviewed four specialist staff and two primary care staff working in NHS Lanarkshire. In these interviews, we used a visual tool (see image on right) based on the ‘donut’ model of care (see figure above) to capture their perspective of the primary and secondary care system, with the people they support who are living with type 2 diabetes in the centre. Participants were asked to place themselves on the map, and tell us about their role and the kinds of people they support. We also mapped all the staff they collaborate with, conversations, tools and challenges they experience in their role. The interviews lasted around one hour, and took place at the participant’s workplace. In addition, we also interviewed staff who designed and deliver the current structured education programme in Lanarkshire.
Interviews with people living with type 2 diabetes
Credit: Louise Mather, No Middle Name, 2019
We interviewed four people living with type 2 diabetes in Lanarkshire. During the interview, we used a similar visual tool to the one used in interviews with staff, adapted to map the participant’s experience of the current service, any challenges, and ideas for how things could be improved. Within the interviews we specifically asked participants to recall their experience of diagnosis. The interviews were relaxed and informal, lasted around one hour, and took place wherever was convenient for the participants. We also audio recorded and transcribed the interviews with the participant’s consent.
POP-UP ENGAGEMENT
Credit: Gemma Teal, 2018
We visited the diabetes clinics at University Hospital Hairmyres and University Hospital Monklands for two half-day pop-up engagement sessions. Stationing ourselves at the entrance to the clinics, we asked participants two questions:
What keeps you well?
What was the most valuable information you received at diagnosis or something you now know that you wished you had been told at diagnosis?
Responses were written on card apples that were added to a freestanding tree. These engagements gave us the opportunity to talk to people living with type 2 diabetes who receive specialist care to gather their feedback on how to improve the diagnosis experience based on critical reflections of their own care journey.
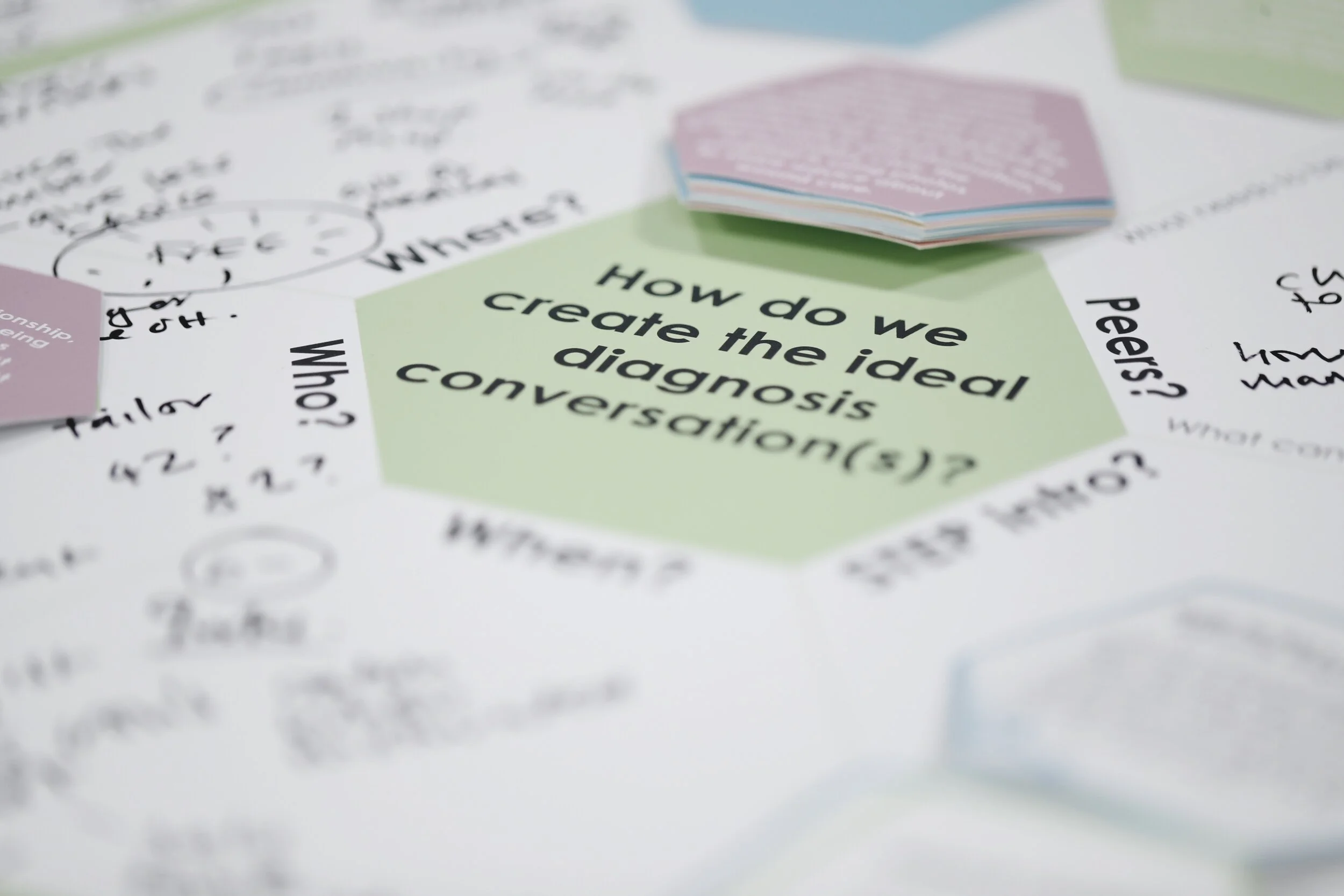
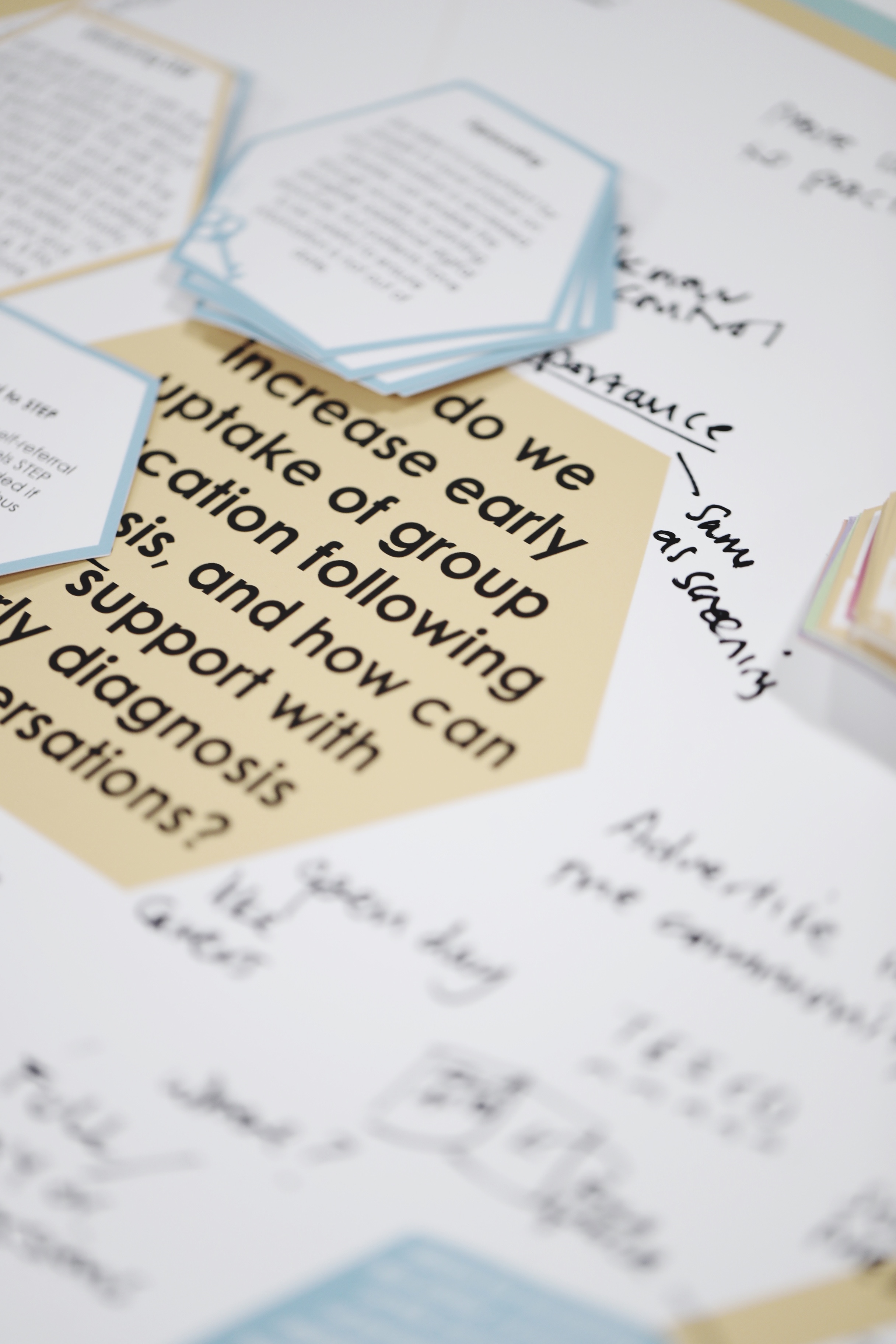
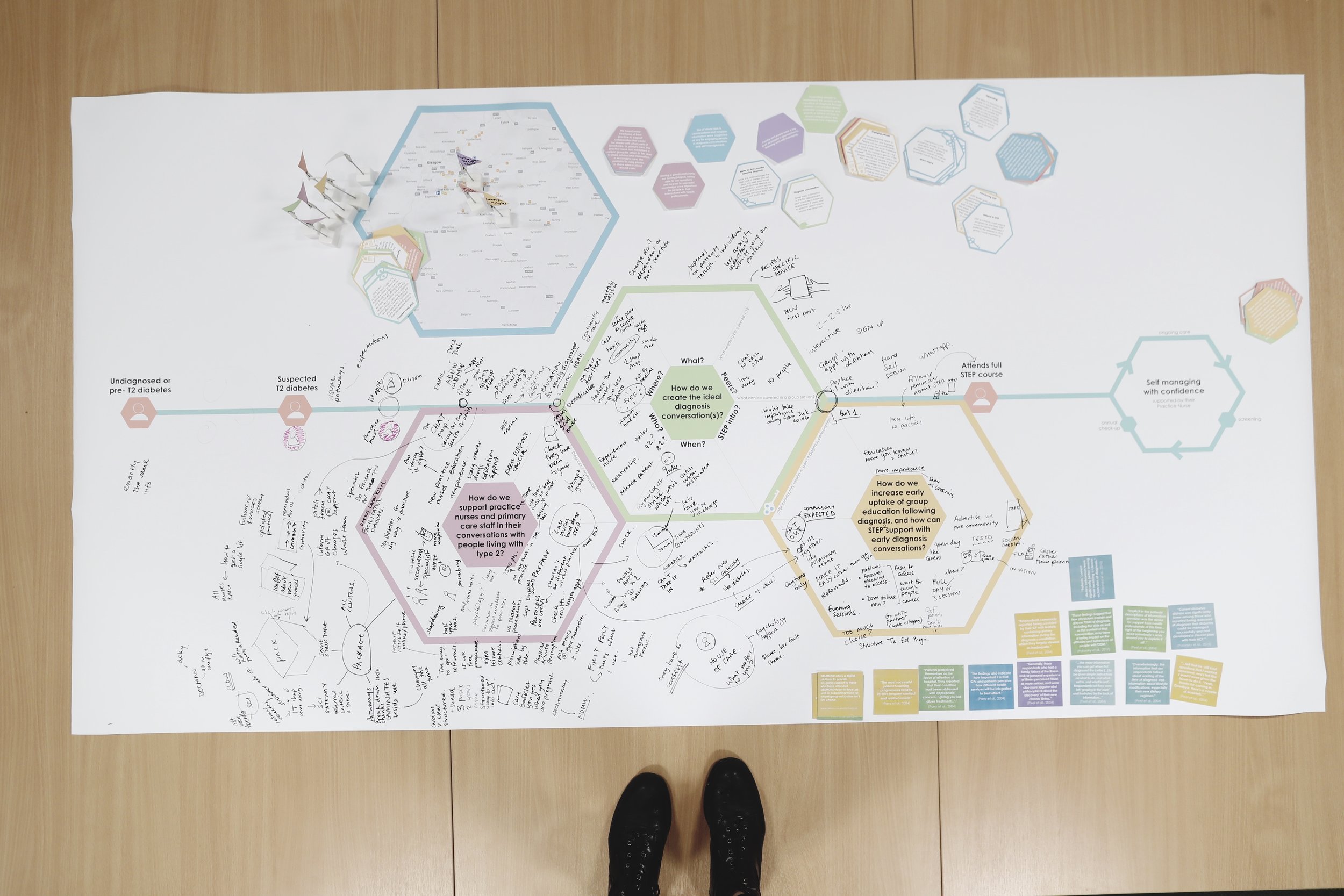
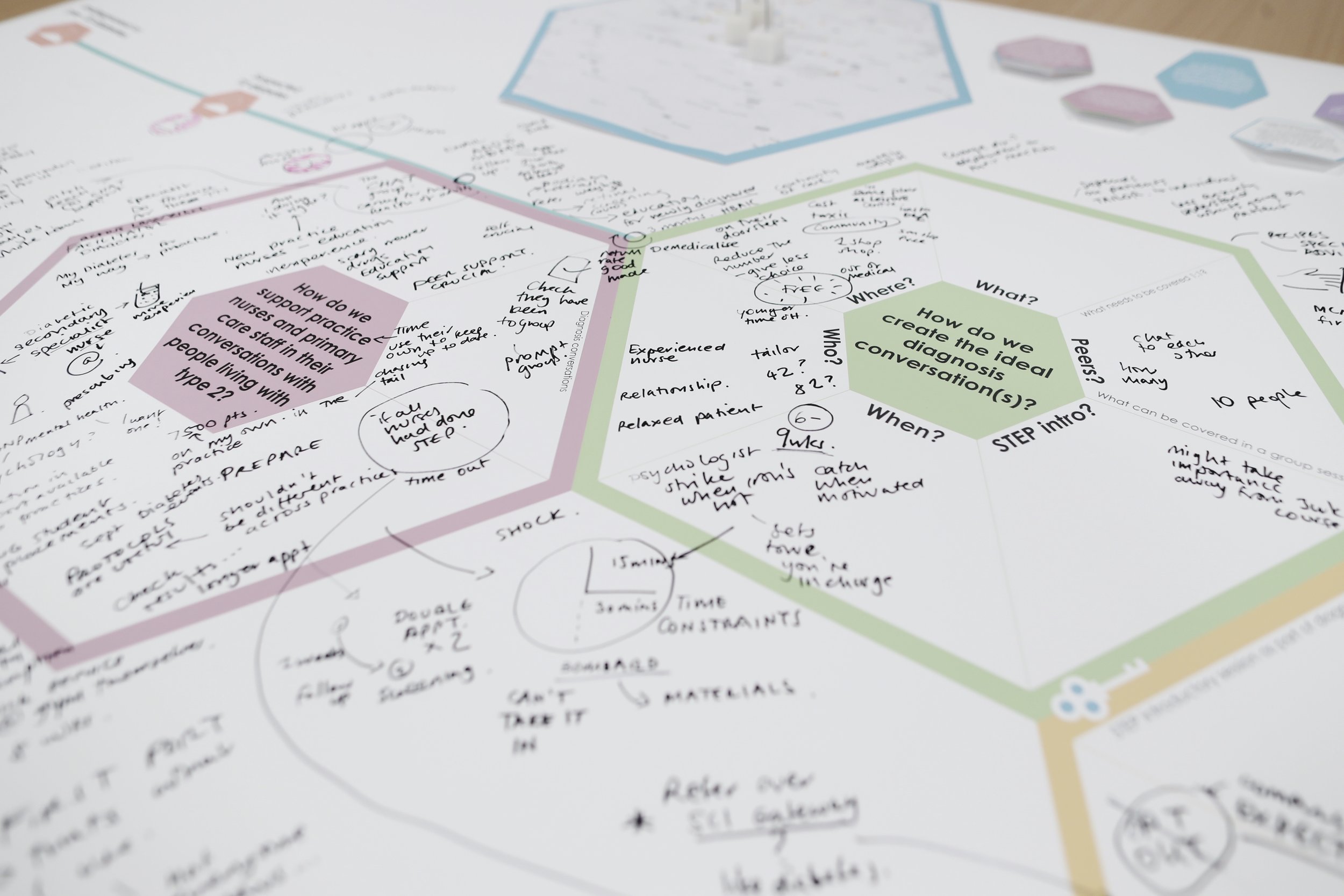
CO-DESIGN WORKSHOP
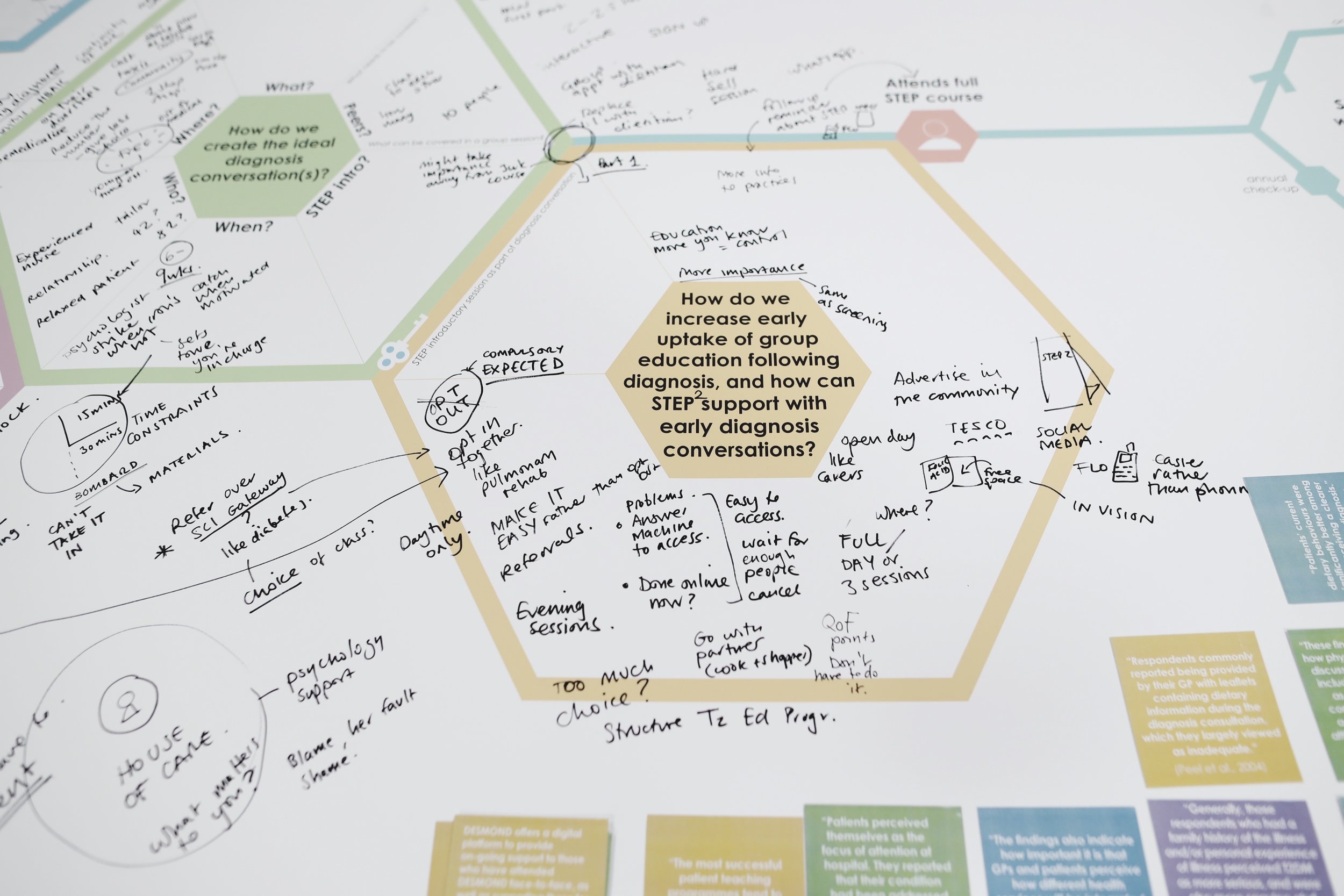
The transcribed interviews and pop-up engagement responses were thematically analysed to identify insights to support redesign of the diagnosis experience, presented in full in an Interim Report (available for download via the links at the bottom of this page) and summarised below. The findings identified three focus areas for a co-design workshop with practice nurses (n=8) and diabetes specialists (n=2). These represented opportunities to innovate the experience of diagnosis and ways of working across the primary and secondary care interface. The focus areas were introduced to participants of the co-design workshop using a specially designed tool which plotted the opportunities along a typical care journey of a person diagnosed with type 2 diabetes. The opportunities were framed as questions, supported by relevant insights or ‘key ingredients’ from our interim findings to inform and inspire participants:
How do we create the ideal diagnosis conversation – who, what, where, when, how?
How do we increase early uptake of structured education following diagnosis?
How do we support primary care staff in their conversations with people living with type 2 diabetes?
Through a facilitated whole-group discussion we explored the questions and collaboratively developed concepts to innovate the service.
















Credit: Louise Mather, No Middle Name, 2019
Credit: Louise Mather, No Middle Name, 2019
Pop-ups and interviews to test the emerging concepts
The concepts were translated into scenarios for future care, represented visually on large printed boards. Three pop-up events were undertaken across NHS Lanarkshire: University Hospital Hairmyres, University Hospital Monklands and Hunter Health Centre. The concept visualisations were displayed on easels, with space for researchers to note feedback and comments to refine the concepts with input from people attending appointments. A paper prototype of one of the concepts was used to gain specific feedback on the format and layout. The pop-ups were also opportunities to engage with health professionals, and gain feedback from a member of council staff responsible for physical activity and weight management referrals and a wayfinding volunteer. We also took the concept visualisations to gather feedback from three of the interview participants living with type 2 diabetes who we engaged with earlier in the project. The interviews were audio recorded and transcribed, and the feedback was used to further refine the concepts.
Policy Review
In parallel with these activities, the DHI Research and Knowledge Management Team have undertaken policy review and market analysis relating to diabetes services in Scotland. This report can be downloaded, in addition to the full project report via the links at the bottom of this page.
findings
UNDERSTANDING THE CURRENT EXPERIENCE
FROM THE PERSPECTIVE OF PEOPLE LIVING WITH TYPE 2 DIABETES
Participants stressed the importance of early, accurate diagnosis, and support to understand and accept why they have developed the condition. Investing time early on to support people to understand their condition, and ensuring they have all the required information specific to their needs were thought to be key to enabling people to self manage and live well. Pop-up participants expressed the need to communicate the severity of the condition at diagnosis through realistic conversation about potential consequences and practical advice on how to avoid complications. Interview participants who had received their diagnosis in a secondary care setting valued the specialist input received at diagnosis and felt it shaped a better understanding of their condition. Despite this high value placed on specialist advice and peer support, it was clear that some may still choose not to engage because of other reasons.
Interview participants expressed different motivations and triggers for engaging with self management, including the perceived severity of their condition, a fear of complications, or to avoid medications and insulin. For some, the lack of any short term impacts or symptoms was a key reason not to engage. Understanding people’s personal circumstances, internal struggles, expectations and needs from their care were important factors in supporting them to overcome barriers and increase engagement. Having a good relationship, not feeling judged and being able to ask questions were important for people in their interactions with health professionals. In addition, understanding people’s goals (both related to their condition and living well in general) seemed to be key to understanding people’s motivations to self manage.
Insights from interviews and pop-up engagement with people living with type 2 diabetes. (Insights presented in full in the Interim Report, available for download via the links at the bottom of this page)
There was an appetite for specific, practical instructions on the dietary changes people need to make. Providing the reasons for these instructions, explaining why screening is necessary, and showing the impact (e.g. through test results) can help people to prioritise these actions. Tailoring the information to the person’s circumstances and appreciating that they may have other competing challenges can help to ensure they engage with the advice. Use of visual aids in conversations and tangible information were suggested as useful for engaging and informing people in the diagnosis conversation. Having access to tools and services that can offer additional information and support was seen to be important to enable people to have greater control in managing their condition. In general, leaflets were thought to be lacking in quality, and access to or motivation to use online resources was limited among some of the participants.
An interview participant who had attended group education found reassurance in meeting others with the same condition, and learned from other’s questions. Other participants talked about how friends who were also living with diabetes had supported them, and suggested hearing stories of other’s experiences would be useful for newly diagnosed people.
FROM THE PERSPECTIVE OF HEALTH PROFESSIONALS
The diagnosis conversation and changes in the person’s condition were seen as key opportunities to motivate and encourage people to make lifestyle changes. The importance of offering reassurance, positive messages and time to digest the information were approaches used to leverage these opportunities. While some staff talked about their responsibility to support the person to self manage, others felt people living with type 2 diabetes need to take more responsibility for their own care.
Understanding the factors that prevent engagement, being realistic that people will relapse, understanding the impact of family and agreeing personal goals were all seen as useful approaches. Being honest and direct, and sharing practical and specific advice about diabetes was seen to be important. Checking the person has understood the key messages from the conversation was seen as a way of ensuring the information is getting across.
Structured group education was seen to be a fantastic resource to support self management, but challenges were identified in encouraging people to attend, leading to poor uptake. We learned that the NHS Lanarkshire structured education programme for type 2 diabetes (STEP 2) is currently being prepared for accreditation by the Scottish Government. Information and education from other sources were also seen as valuable and popular with people living with type 2 diabetes. We learned about successful initiatives that offer referral to community-based services (e.g. Weigh to Go) that are seen to be popular with people living with type 2 diabetes.
Staff discussed some of the challenges people living with type 2 diabetes experience in terms of: apprehension of going to see specialist staff, difficulties in discussing and understanding long-term complications when there are no short-term signs of the condition, and the lack of psychological support.
Insights from interviews and pop-up engagement with health professionals. (Insights presented in full in the Interim Report, available for download via the links at the bottom of this page)
Collaboration between primary care and specialist staff
Examples of collaborative working across the primary and secondary care interface were shared, and tended to be most evident in places where specialist and primary care staff were co-located. In some areas, opportunities for communication between primary and specialist staff were very limited. While some practice staff used parts of SCI-Diabetes to access information, the lack of integration with primary care systems meant that they did not use it to add information about their consultations to allow joined-up care.
Keeping up-to-date with new guidelines, treatments and approaches through e.g. attendance at diabetes conferences was seen by some as part of ensuring they were delivering the best possible care for people living with type 2 diabetes. Not having sufficient time to get up to date with new practice and make changes was seen as a barrier to implementation. We learned about variation across primary care in Lanarkshire in terms of the time available for diagnosis appointments and follow ups, support from the wider GP team and awareness or use of the available resources for diabetes. It was clear that staff who felt supported by their employers, and who made a concerted effort to look after their own health and wellbeing felt better able to cope with the demands of their job. In primary care, one practice nurse had established a support group with others in her area to share advice, information and peer support. We also learned that there is an aspiration to work more closely with local community-based services and create stronger links between programmes such as Weigh to Go and STEP 2 structured education to ensure joined-up care and supported self management.
Opportunities to Innovate
Three clear focus areas to innovate the experience of diagnosis and ways of working across the primary and secondary care interface emerged from the interim findings. These were framed as questions, to be explored with primary care and specialist staff in a co-design session:
How do we create the ideal diagnosis conversation – who, what, where, when, how?
How do we increase early uptake of structured education following diagnosis?
How do we support primary care staff in their conversations with people living with type 2 diabetes?
future service
the new diagnosis experience
Concepts are presented for a new visual tool to support the diagnosis conversation, a new diagnosis group education appointment with a specialist, and new ways of working across primary and secondary care to support practice nurses to deliver person-centred care. Each concept is prefaced by the insights that inspired them, a detailed description of the concept that emerged from the co-design workshop, and a discussion of the feedback received during pop-up engagement and interviews with people living with type 2 diabetes.
These concepts together form the new diagnosis experience, which is discussed alongside recent developments in diabetes policy at a national level. In addition to this ‘near’ future map, we present a future vision for care enabled by new digital services and a roadmap to support discussion and further development towards implementation.
concept 1: diagnosis conversation tool
Insight
Some participants living with type 2 diabetes told us that there was a lot to take in during their diagnosis conversation, making them feel overwhelmed. This can make it difficult to navigate and understand the different appointments in the period after diagnosis. Experienced practice nurses told us they keep a ‘cheat sheet’ on their desk as a reminder of the many different things they need to cover in a new diagnosis appointment. They worried that some people were not able to take everything in during the first appointment, particularly when they were dealing with the stressful news that they had a long-term condition.
Both people living with diabetes and practice nurses told us that information about the long-term consequences of diabetes can be challenging to get across, but that it is vital that people understand the importance of managing their condition. In addition, both groups highlighted the power of visual aids in conversations to support people to engage and understand. They contrasted this with leaflets and information sheets that often contain a lot of text, which can be overwhelming.
CONCEPT
Introducing a new paper-based tool to support the diagnosis conversation. The tool structures and records the conversation between the practice nurse and the newly diagnosed person, and ensures consistency of experience and messages across practices. It has been designed to structure and prompt key aspects of the conversation:
Building a relationship: the front page invites the practice nurse to explain their role and invite the person to contact them if they have any questions or issues.
Planning care: inside, the booklet uses icons printed as stickers which can be added to the care pathway visual to produce a personalised care plan. There is plenty of white space around the visual to permit the nurse to make notes. This can be reviewed and updated as required.
Shared-decision making: the practice nurse can chat through the options before they decide on what is right for the person.
Visual summary: the supporting information acts as a key for the care plan, explaining what each icon represents and referring to the page number of the new standardised NHS Lanarkshire type 2 diabetes information pack for more detailed information. It also functions as a memory aid to support the practice nurse to cover key information about the services and support available.
Navigating the early stages post diagnosis: using the visual care pathway, the practice nurse can reassure the person that although the first few months can feel demanding with numerous appointments, this will settle down.
Long-term complications: using the circular part of the pathway, the practice nurse can discuss the purpose of screening and relate it to the importance of managing their condition to avoid complications.
Goal planning: discussing their personal goals can also be used as away to understand what is important to the person in the longer-term, and use this to help tailor their care and conversations about lifestyle changes they may need to make to achieve this, e.g. if they can reduce their HbA1C through lifestyle changes they can avoid starting medication.
Documentation: the plan can be scanned to provide a short digital summary of what was discussed for the practice nurse’s records, with the hard copy given to the person to take-away as a reminder of what was discussed.
Practice nurses stressed the importance of developing this new tool through engagement with all practices in Lanarkshire to ensure it addresses variation, achieves acceptance and becomes embedded in practice.
FEEDBACK
As a result of feedback from people living with type 2 diabetes, the prototype was reduced in size to make it more portable, and the textual content was reduced to simplify the design. A pocket was added to the tool to store the stickers and potentially a card with a print out of their results to support the discussion (see image above).
Both health professionals and people living with type 2 diabetes felt the tool could help to improve the overall diagnosis experience. One of the participants felt that it would help to flag things if anything was missed (e.g. if they did not receive a screening appointment). Another participant noted that having the plan would help to join up the care and avoid overlaps (e.g. separate eye screening at the GP practice, hospital and ophthalmologist). They also felt the tool could also help to increase awareness of local services, most of which are free to access (e.g. healthy walking, managing stress).
It was emphasised that for the tool to work, resources need to be in place to deliver the care plan.
concept 2: Diagnosis Specialist Group Appointment
Insight
Some people living with type 2 diabetes told us they would like more specialist input early on in their journey. Early education and peer support were found to be important for engaging people in self management. Health professionals highlighted that some people are reluctant to attend a 1:1 appointment with the dietitian due to stigma or fear of being judged on their eating habits. People who have attended the STEP programme highlighted its benefits and said that they wish they had been aware of the programme earlier.
CONCEPT
Introducing a group education appointment within 6-9 weeks of diagnosis was suggested as a way to ensure early access to specialist input, and increase uptake of the full STEP 2 structured education programme. This would be an alternative to the current 1:1 appointment with the specialist dietitian – by seeing patients in small groups the dietitians felt this would make a more efficient use of their time. The person would be referred for this appointment by the practice nurse during the diagnosis conversation using the same process they currently use to refer to the dietitian. Specialist diabetes educators advised that this session should last around two hours, and include some interactive activities based on the principles of adult learning. The sessions could be scheduled for regular days and times in a range of different accessible community locations to increase availability and reduce waiting times for structured education. At the session, the person could choose to sign up for the full STEP 2 structured education or to receive a text message reminder to sign up at a later date.
FEEDBACK
Specialist staff and practice nurses felt that this could be an important step towards addressing the gap in access and uptake of structured education, and equip more people with the information and tools to self manage early on to reduce the risk of complications. Some staff felt that it would be more feasible to organise the group appointment within 12 weeks of diagnosis. People living with type 2 diabetes agreed that early specialist input and education is important, and emphasised that it is only effective if it happens soon after diagnosis, again referring to capacity issues and off-putting waiting times.
CONCEPT 3: SUPPORT FOR PRACTICE NURSES
INSIGHT
There are variations in patient pathways and the support available to practice nurses across Lanarkshire. This included variation in the time available to devote to diabetes diagnosis conversations. Some practice nurses are able to allocate 30 minutes and take time to review the person’s results and prepare prior to the appointment, while others are restricted to 10-15 minutes with no preparation time. Addressing these through enabling greater collaboration between primary care and specialist staff, offering more learning support for practice nurses and raising awareness of best practice throughout the wider GP team were highlighted as key to ensuring consistency of the new diagnosis experience.
CONCEPT
During the co-design workshop, practice nurses shared many ideas for new forms of support. They suggested that attending the new diagnosis specialist group appointment (see concept 2) would be a great way to learn about new developments and the benefits of structured education so they can promote this to their patients. For new practice nurses, shadowing more experienced nurses and having specialists observe some of their diagnosis appointments and give feedback would ensure they felt confident in the quality of their care. In response to challenges in communication between primary and specialist care, they suggested creating a network and email list to disseminate messages and updates.
They highlighted the need for support sessions for practice nurses across Lanarkshire to share working practices and resources, and receive training and updates from specialist staff. They also saw this as an opportunity to involve practice nurses in any future developments (e.g. the development of the new conversation tool and the standardised information pack) to ensure they meet their varying needs. They highlighted the need for specialist staff to engage with the wider GP team to ensure consistency and support for the practice nurses at a local level. While there was a real appetite for input from specialist diabetes staff through training and development sessions, practice nurses cautioned that they have very limited time to spare and are often forced to do these kinds of activities in their own time.
OVERVIEW of the new service
Credit: Sneha Raman, 2019
All illustrations adapted from an image bank created by Tessa Mackenzie, 2018
These concepts together form the new diagnosis experience, which aligns with ongoing developments in NHS Lanarkshire and key priorities set out in diabetes policy at a national level, as detailed in the visual below.
Credit: Sneha Raman and Gemma Teal, 2019
Note: This visual references the ‘A Healthier Future – Framework for the Prevention, Early Detection and Early Intervention of type 2 diabetes’ recently published by the Scottish Government (2018)
ROADMAP TO FUTURE SERVICES
The next steps for NHS Lanarkshire to implement the new diabetes diagnosis experience are set out here, presenting a roadmap to the ‘near’ future service, alongside a medium-term future vision of care enabled by new digital services. This roadmap is intended as a discussion tool to understand how we can support implementation of the new diagnosis experience, and to enable scoping of future opportunities for collaboration with NHS Lanarkshire and across Scotland.
Acknowledgements
We would like to thank all of our interview participants for giving up their valuable time and for generously sharing their stories to inspire service redesign.
We would also like to thank the diabetes team across NHS Lanarkshire for supporting recruitment of interview participants and recruitment of NHS staff for co-design workshops.
Finally, many thanks to staff at University Hospital Monklands, University Hospital Hairmyres and Hunter Health Centre for permitting and facilitating our pop-up engagement sessions in their busy clinic foyers, and to all the citizens and staff who engaged with us to share their views.
download the report
Download the final report of this project, or the summary report:
Final Report: Print friendly A4 (coming soon)
Policy Review (coming soon)
Further Information
For more information about this project please contact:
Sneha Raman, S.Raman@gsa.ac.uk
Gemma Teal, G.Teal@gsa.ac.uk